BACKGROUD
HIV infection leads to T cell dysfunction, which triggers increased incidence of diffuse large B cell lymphoma (DLBCL). It has been shown that PD-1 inhibitors can better restore T cell function and effectively treat HIV-related lymphoma. However, the specific mechanism on the treatment of HIV-related DLBCL patients with PD-1 inhibitors is ambiguous, and related studies on the expression of PD-1 on T cells have not been reported. This study aimed to explore the regulatory role of altered immune function status in the microenvironment of HIV-related DLBCL and to analyze hyper-exhausted T cell subsets.
METHODS
Three patients with DLBCL, two patients with HIV and 11 patients with HIV-related DLBCL who were treated from September 2021 to December 2022 at the Chongqing University Cancer Hospital of were included. Single cell sequencing was used to analyze immune cell and tumor cell related genes in patients'lymph node tissues. InferCNV was used to distinguish normal and malignant B lymphocytes. Gene set enrichment analysis (GSEA) was used to find the expression of exhaustion genes and related signaling pathways in immune cells. And relevant exhausted immune cells were analyzed and validated by flow cytometry.
RESULTS
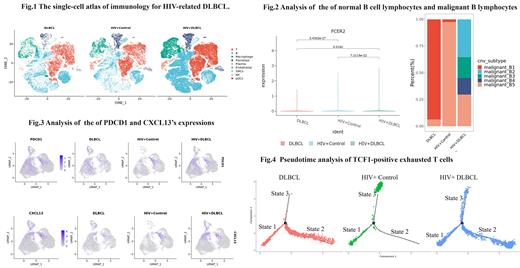
Compared to the HIV and DLBCL groups, the HIV-related DLBCL group had a higher level of expression of the gene PDCD1, a higher level of expression of CD23(FCER2) in normal B lymphocytes, and a greater difference in malignant B lymphocytes, with a lower percentage of TCF1-positive exhausted T cells and a higher level of CXCL13-positive exhausted T cells (Fig.1-3). Compared with the HIV group, the percentage of follicular helper T cells (T fh) was lower in the HIV-related DLBCL group. The results of the Pseudotime analysis showed two main developing directions of TCF1-positive exhausted T cells (Fig.4). The state2 was primarily the direction of TCF1-positive exhausted T cell development in the HIV group and the HIV-related DLBCL group, and the state3 was primarily the direction of TCF1-positive exhausted T cell development in the DLBCL group and the HIV-related DLBCL group.
CONCLUSION
Patients with HIV-related DLBCL are more at risk of T cell exhaustion. In this study, we found that HIV-related DLBCL induced T cell exhaustion has different states and shows two differentiation directions, and state2 may correlate with HIV-induced T cell exhaustion. T cell exhaustion states may be used for disease status and clinical efficacy assessment of HIV-related DLBCL.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal